Now here is another interesting case presented by Dr Hitesh and Dr Anuraga in the post https://hitesh116.blogspot.com/2020/05/12may-2020-elog-medicine-intern.html?m=1

An 18 year old patient came with the following chief complains:
- Weakness of both lower limbs since 20 days
- Bilateral edema in lower limbs.

Differential diagnosis
At birth
- None as systemic causes; mainly hereditary
Onset in childhood
- Inflammatory myopathies – dermatomyositis, polymyositis (rarely)
- Infectious myopathies
- Endocrine and metabolic disorders – hypokalemia, hypocalcemia, hypercalcemia
Onset in adulthood
- Inflammatory myopathies – polymyositis, dermatomyositis, inclusion body myositis, viral (HIV)
- Infectious myopathies
- Endocrine myopathies – thyroid, parathyroid, adrenal, pituitary disorders
- Toxic myopathies – alcohol, corticosteroids, narcotics, colchicines, chloroquine
- Critical illness myopathy
- Metabolic myopathies
- Paraneoplastic myopathy
Laboratory Evaluation for Suspected Myopathy
Confirm the Presence of Muscle Disease
Identify Etiology
Suspected Inflammatory Etiology
- Myositis-specific autoantibodies
- Anti–double stranded DNA antibody
- Anti-Scl 70 antibody
- Anti-SSA and SSB antibodies
- Anti-ribonucleoprotein antibody
- Rheumatoid factor
- Anti-PM1 antibody
- Angiotensin-converting enzyme levels
Suspected Mitochondrial or Metabolic Myopathy
Suspected Amyloid Myopathy
- Immunofixation electrophoresis of monoclonal proteins in serum and urine.
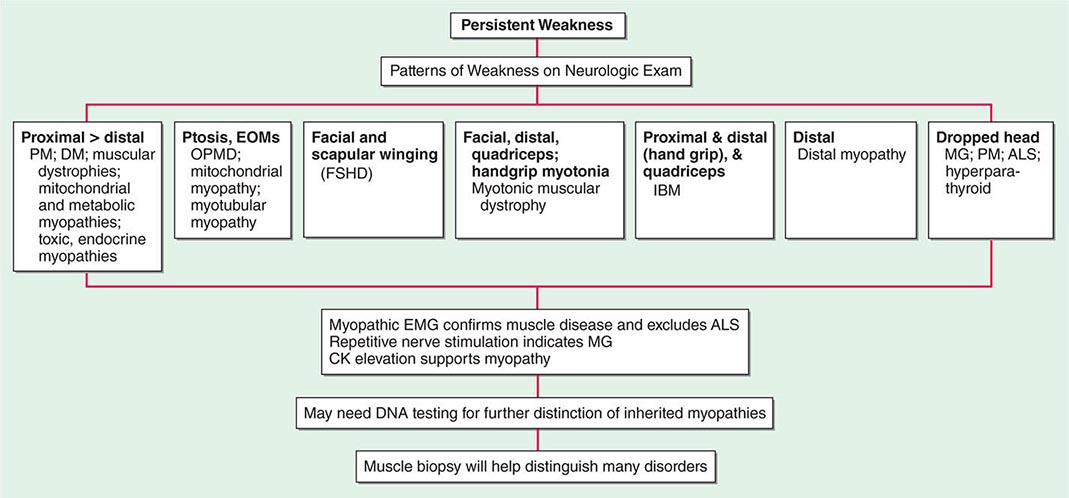
Based on the involvement of proximal limbs and then later distal and based on muscle biopsy report showing adipocytes, atrophic or necrotic muscle fibres suggesting muscular dystrophy on the basis of following criteria:
- Lymphedema
Lymphedema is a condition that makes it difficult for lymph fluid to properly drain due to a blockage. It’s often caused by a surgical procedure or as a secondary condition. You can also be born with it.
When lymph fluid can’t drain it accumulates and causes swelling. Lymphedema can be either pitting or non-pitting.
- Myxedema
Some people with severe or advanced hypothyroidism develop a condition called myxedema. It tends to cause swollen legs and feet, but it can also cause swollen eyelids and lips. In some cases, it can also cause tongue swelling.
- Lipedema
Lipedema causes fat cells to grow and proliferate, and leads to increased fluid retention around the cells which results in non-pitting edema that’s often tender or painful. It usually affects the legs and feet and occurs almost exclusively in women.
HOW TO DIAGNOSE????
- Lymphedma-can be diagnosed with a simple basic physical examination
- Myxedema -can be detected by thyroid profile-T3 , T4, and TSH levels
- Lipedema-physical signs, such as:
Treatment
Lymphedema treatments
Lymphedema usually responds well to complex decongestive therapy (CDT). This involves:
- using gentle massage to stimulate fluid movement and open up lymphatic capillaries
- wrapping the area with bandages
- following a skin care routine to keep the affected area moisturized
- getting regular exercise
- wearing compression garments
Lipedema treatments
While there’s no treatment for lipedema, many people find that CDT also works well for lipedema symptoms. Lipectomy, a modification of liposuction, may also help with lipedema in its earlier stages.
Myxedema treatments
Myxedema usually requires medication, such as a synthetic T4 hormone called levothyroxine. This will help to restore the balance of your thyroid hormones. Keep in mind that it may take a few weeks for this treatment to start working.
Other findings
- Raised urea, creatinine and uric acid levels

- It suggests some kidney pathology
- but raised creatinine also indicates Muscular dystrophy.....it has been found that creatinine levels were significantly higher in BMD (Becker muscular dystrophy )patients in comparison to DMD ( Duchenne muscular dystrophy )patients, indicating that a higher serum creatinine level is linked to a milder disease
Treatment
- There is no cure, but treatments are available to help with symptoms and maximize muscle function
- Treatment can also include genetic counseling, using splints, massages, and catabolic steroids.
- but the use of glucocorticoids has not been adequately studied in Becker dystrophy.
Comments
Post a Comment